- Research
- Open access
- Published:
Impact of interventions to reduce nosocomial transmission of SARS-CoV-2 in English NHS Trusts: a computational modelling study
BMC Infectious Diseases volume 24, Article number: 475 (2024)
Abstract
Background
Prior to September 2021, 55,000–90,000 hospital inpatients in England were identified as having a potentially nosocomial SARS-CoV-2 infection. This includes cases that were likely missed due to pauci- or asymptomatic infection. Further, high numbers of healthcare workers (HCWs) are thought to have been infected, and there is evidence that some of these cases may also have been nosocomially linked, with both HCW to HCW and patient to HCW transmission being reported. From the start of the SARS-CoV-2 pandemic interventions in hospitals such as testing patients on admission and universal mask wearing were introduced to stop spread within and between patient and HCW populations, the effectiveness of which are largely unknown.
Materials/methods
Using an individual-based model of within-hospital transmission, we estimated the contribution of individual interventions (together and in combination) to the effectiveness of the overall package of interventions implemented in English hospitals during the COVID-19 pandemic. A panel of experts in infection prevention and control informed intervention choice and helped ensure the model reflected implementation in practice. Model parameters and associated uncertainty were derived using national and local data, literature review and formal elicitation of expert opinion. We simulated scenarios to explore how many nosocomial infections might have been seen in patients and HCWs if interventions had not been implemented. We simulated the time period from March-2020 to July-2022 encompassing different strains and multiple doses of vaccination.
Results
Modelling results suggest that in a scenario without inpatient testing, infection prevention and control measures, and reductions in occupancy and visitors, the number of patients developing a nosocomial SARS-CoV-2 infection could have been twice as high over the course of the pandemic, and over 600,000 HCWs could have been infected in the first wave alone. Isolation of symptomatic HCWs and universal masking by HCWs were the most effective interventions for preventing infections in both patient and HCW populations. Model findings suggest that collectively the interventions introduced over the SARS-CoV-2 pandemic in England averted 400,000 (240,000 – 500,000) infections in inpatients and 410,000 (370,000 – 450,000) HCW infections.
Conclusions
Interventions to reduce the spread of nosocomial infections have varying impact, but the package of interventions implemented in England significantly reduced nosocomial transmission to both patients and HCWs over the SARS-CoV-2 pandemic.
Introduction
Over the course of the COVID-19 pandemic in England, there has been evidence of nosocomial SARS-CoV-2 transmission to both patients and healthcare workers (HCWs) [1,2,3,4], with 0.5–1.25% of susceptible inpatients (55,000–90,000 patients) identified as having developed a nosocomial infection between 01-March-2020 and 01-Sept-2021 [5, 6]. Several interventions have been introduced in hospitals to reduce the transmission rate of SARS-CoV-2 including regular testing of patients and HCWs, increased hand-hygiene, and HCWs wearing masks/face coverings universally (i.e., around both patients and HCWs), in addition to hospital system changes such as reductions in occupancy [7, 8]. It is difficult to assess the effectiveness of individual interventions through data-driven approaches alone because several measures were implemented in quick succession. The emergence of vaccines and new variants have also altered nosocomial transmission rates over time, providing further uncertainty [5]. Computational modelling can help address these issues by providing a framework where individual interventions can be removed/reversed individually or in combination, counterfactual simulations can be executed, and the effectiveness of interventions assessed [9]. Using a previously developed computational model [10] we present an estimate of the impact of interventions in place during the pandemic, provide a counterfactual analysis of what might have happened had they not been implemented, and predict which combinations of interventions have the highest impact on transmission to both patients and HCWs.
We estimated the impact of eight hospital interventions/changes on nosocomial infections in both patients and HCW by 1) combining evidence from the literature on the efficacy/effectiveness of individual measures for reducing the spread of respiratory viral infections in hospitals and the community; 2) modifying model parameters to reflect scenarios in which the interventions were ‘reversed’ (both individually and collectively), e.g., through modifying the probability of transmission from inpatients and HCWs; and 3) modelling counterfactual scenarios in which interventions were ‘reversed’, i.e., simulating the hypothetical scenario in which the interventions/changes had not been implemented, to estimate how much virus transmission and resulting infections they averted individually and when combined.
Methods
Model development and calibration
We have extended an existing individual-based model (IBM) of nosocomial transmission within and between patient and HCW populations [9, 10]. The model simulates transmission through different routes: i) patient-to-patient transmission between those sharing a bay, ii) patient-to-patient transmission between patients residing on the same ward but not necessarily in the same bay, representing transmission through, for example, fomites, shared facilities, or transient asymptomatic carriage by HCWs, among others, iii) patient-to-HCW transmission, iv) HCW-to-patient transmission, v) HCW-to-HCW while present on the same ward, and vi) HCW-to-HCW anywhere in the hospital. Indirect transmission is captured implicitly in the model as a result of transmission occurring on wards between any HCWs that have shared a space within a 4 h time step (and so in practice may not have occupied that space concurrently) and through the indirect transmission route whereby HCWs anywhere in the hospital may infect other staff with no explicit requirement for them to physically share a space at any time. Infected patient cases are imported from the community at a rate calculated from observed hospital admissions in the NHSE Situation Report data [6]. HCWs can become infected in the community when they are outside of the hospital according to the predicted community prevalence on that date, where the prevalence was calculated from the Cambridge Real-Time Model [11]. Under the baseline scenario, the IBM is parameterised using multiple national datasets and values from the literature and is calibrated to reproduce the transmission dynamics of SARS-CoV-2 among healthcare workers (HCWs) and patients in an average English hospital. A full model description and details of the calibration procedure are described in Supplementary File 1.
Counterfactual modelling of ‘reversal’ of interventions
Counterfactual scenarios were simulated in which eight interventions were reversed (individually and collectively) and compared to a baseline where interventions were in place, with scenarios as follows: 1) Baseline – transmission and interventions simulated to reflect observed numbers of infections in the data; 2) removal of lateral flow device tests (LFDs) for HCWs that were introduced in November 2020; 3) reversal of improvements in hand-hygiene from the start of the pandemic; 4) reversal of testing and cohorting of symptomatic patients throughout the simulation period; 5) reversal of reduced occupancy, instead with occupancy remaining at 2019 levels March to May 2020; 6) reversal of suspension of visitors to hospital patients (March to October 2020); 7) removal of universal mask wearing by HCWs (i.e., HCWs wear masks around patients but not around other HCWs) from June 2020; 8) removal of mask wearing by HCWs when treating patients (i.e., HCWs do not wear masks around patients or other HCWs) throughout simulation period; 9) isolation of symptomatic HCWs removed throughout simulation period, 10) reversal of all interventions in 2–9 collectively. The reversal of interventions was parameterised through literature searches and expert elicitation where there was a paucity of evidence (Table 1, Supplementary File 2). A supplementary analysis was also performed exploring a further set of counterfactual scenarios where interventions were in place from the start of the pandemic instead of being introduced at different times as in reality.
After obtaining data for parameterising the reversal of interventions, new parameter sets were generated using the procedure described in Fig. S1 and the Spartan R package [20]. The steps are i) 10 unique baseline transmission parameter sets were drawn from previous model calibrations [10], ii) for each intervention scenario 100 new parameters were generated by sampling 100 unique parameter values from the distribution of the combined study data, iii) each set was mapped to one of the unique 10 transmission parameter sets to produce 100 new parameter sets. To reverse interventions where there was a single value, e.g., increased occupancy, each baseline transmission parameter set was replicated 10 times and then modified to include the single new parameter value in all sets.
These new parameters were used within the IBM to generate estimates of the impact of each intervention individually (in terms of nosocomial infections averted in inpatients and in HCW) as well as an overall estimate of the combined impact of all interventions that were implemented during the COVID-19 pandemic in England.
The model was simulated for 5100 timesteps covering a time period of 850 days from 03-March-2020 to 30-June-2022 (6 steps per simulated day). Individual-level patient and HCW data on infection status and location were recorded at each time step.
Predictive modelling of the impact of combinations of interventions on infection rates
In a further analysis to explore the effect of intervention combinations, a list of all possible combinations of interventions described above was generated (255 total) and then explored. Unlike the previous analysis where vaccines and variants emerged during the pandemic and interventions were put in place at times specified by policy, here we restrict simulation to a 12-week Omicron-like period where the prevalence ranged from 2–4% (similar to January 2022), assuming no protection from previous infection or vaccination. This time period was selected to provide enough time to observe the effect of interventions while maintaining stable prevalence levels in line with community estimates. In this analysis all interventions were removed and then added back either singularly or as part of a package. Simulations were parameterised to reflect the hypothetical removal of all interventions except those included in the combination i.e., in a scenario where patient testing and LFD testing of HCWs were included, all other interventions are reversed as described in Table 1. Parameter files were generated as described above. The results of these simulations were then fed into a linear regression model to estimate the overall impact of each intervention. A second model was used to estimate the impact of combinations of the interventions that were significantly associated with a decrease in the number of infections in model 1.
Results are presented as the number of susceptible inpatients and patient-facing HCWs becoming infected with SARS-CoV-2 under each intervention scenario across the simulation period. To scale up the single-hospital simulation estimate to a national level, the total number of infections prevented is divided by the total number of beds in the simulated hospital (a proxy for hospital size) and then multiplied by the total number of beds across NHS hospitals in England using national data [15]. This assumes that occupancy was similar between all NHS hospitals.
Results
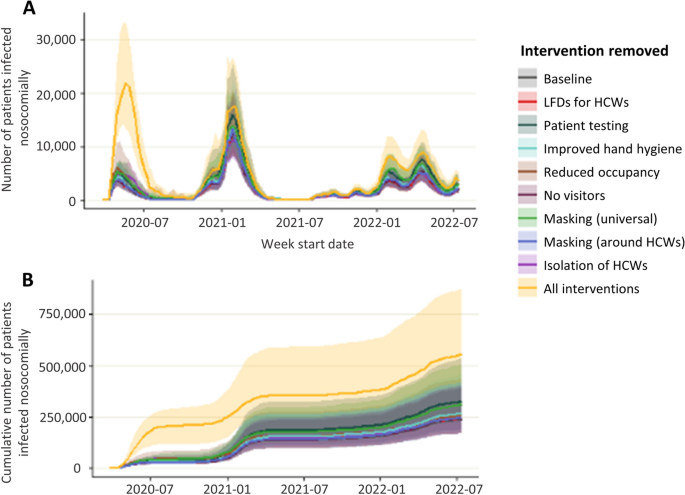
Impact of interventions on nosocomial infections in patients: counterfactual modelling
In the baseline scenario where all interventions were in place, a maximum of 12,300 patients were infected in a single week and 240,000 over the simulation period (March 2020-July 2022, Fig. 1, Table 2, 3.5% of all susceptible admissions). Removing all interventions results in a worst-case scenario of up to 22,000 patients infected in a single week and 560,000 over the simulation period (6.25% %))of all susceptible admissions), a more than two times increase compared to the baseline. The most effective interventions were patient testing and universal masking by HCWs, and removing these interventions resulted in a total of 326,000 and 310,000 patient infections respectively, over the simulation period. Patient testing and universal masking by HCWs were most effective over the omicron wave (from December 2021), and testing was most effective over the first and second waves (March 2020 to May 2021). The least effective intervention overall was restricting visitation: removing this intervention did not result in an increase in infections; however, this intervention was only in place for a short time and therefore only has a limited opportunity for effectiveness (Fig. S2). In a scenario where visitation was restricted throughout the entire simulation period there were 44% fewer patient infections during the omicron wave (Fig. S3). Interventions were most impactful before July 2020 when the wild-type (WT)wave first hit England and between December 2021 and March 2022 when the omicron wave first started. This is demonstrated by the greatest difference between the simulations with no interventions (yellow lines) compared to the baseline (grey lines).
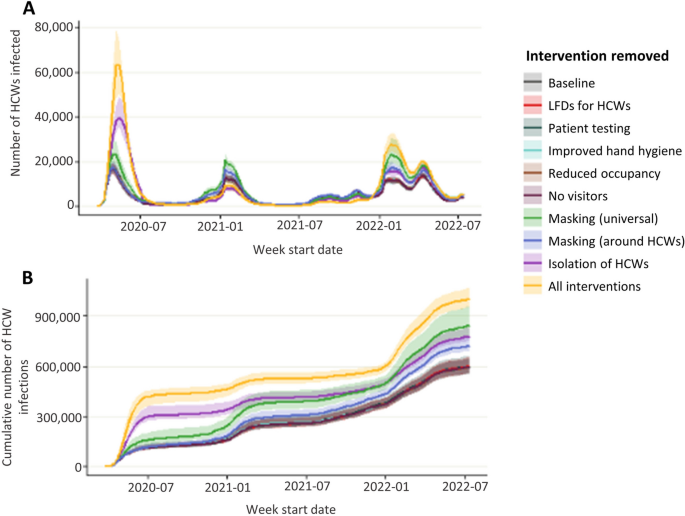
Impact of interventions on HCW infections: counterfactual modelling
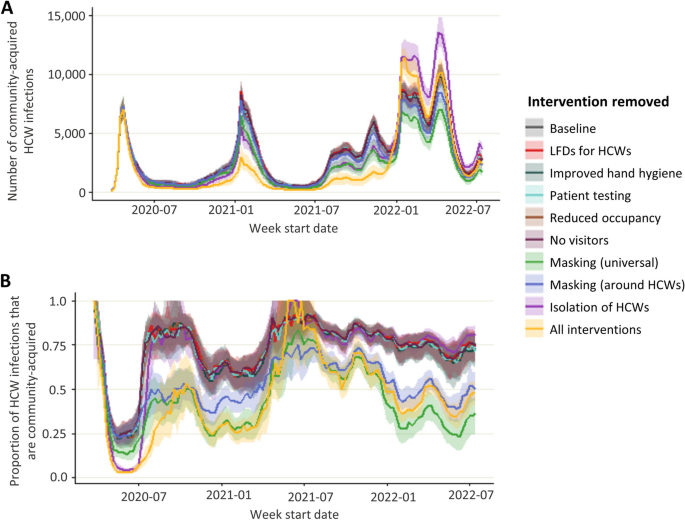
In the baseline scenario where all interventions were in place, a maximum of 17,500 (median, IQR in Table 2) HCWs were infected in a single week and there were 595,000 HCW infections over the simulation period (Fig. 2). When all interventions were removed simultaneously, a maximum of 65,000 HCWs were infected in a single week (10% of all staff) and there were 1 million (0.9 – 1.1 million) infection events in HCWs over the simulation period. The most effective interventions were isolation of symptomatic HCWs, masking universally, and masking around patients. When HCW isolation was removed, up to 40,000 HCWs were infected in a single week, and there were 780,000 infection events in HCWs. Removing masking universally resulted in a maximum of 24,000 HCWs infected in a single week and 850,000 infection events in HCWs. When masking was only in place around patients and not other HCWs a maximum of 18,000 HCW infections in a single week and there was a total of 750,000 HCW infection events. Masking was most effective during the first wave of the pandemic (March – August 2020), and HCW isolation was most effective both during the first wave and also over the omicron wave (from December 2021). When interventions are removed the main risk to HCWs becomes the hospital, with almost 75% of infections in HCWs being hospital acquired in 2022 (Fig. 3). Relaxing interventions switches the balance of infections from the community to the hospital.
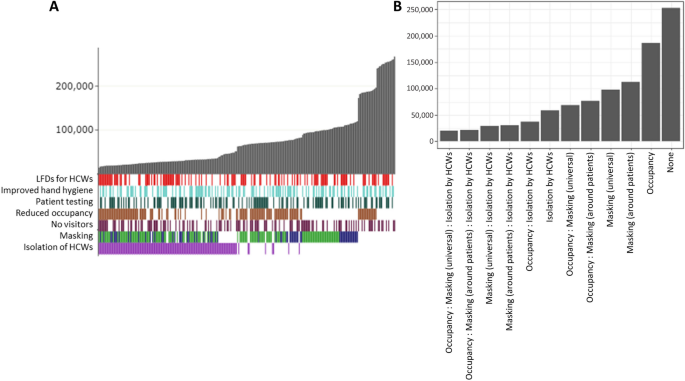
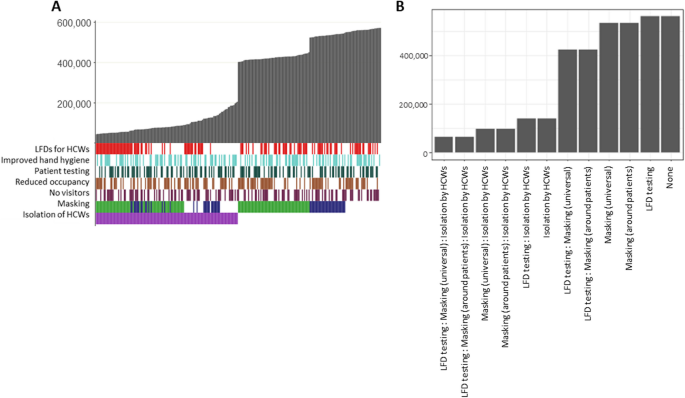
Impact of combined interventions on patient nosocomial infections: predictive modelling
In a scenario with no protection from previous infection or vaccination where all interventions were removed, and then added back in either singularly or as part of a package, restricting visitation as a single intervention was the least effective option, with 270,000 patients nosocomially infected over a three-month period (Fig. 4A). The most effective single intervention was isolation of symptomatic HCWs preventing 81% of infections compared to restricting visitation alone (50,000 vs 270,000). When HCWs testing and isolation upon developing symptoms are in place, both universal masking and masking around patients significantly further reduce infections by up to 25% (36,000 vs 48,000) compared to restricting visitation alone, but there is no clear advantage to universal masking over masking only around patients for preventing nosocomial patient infections. However, when HCWs do not isolate then universal masking has a slight advantage over masking only around patients with an additional 11% reduction in infections (maximum of 107,000 infections when masks are worn universally vs 121,000 when worn only around patients).
Modelled combined effects of interventions on patients. A) Simulated number of patients infected over a 12-week omicron-like period (grey bars) under package of interventions (coloured bars = interventions in package, white = intervention not in package) ordered by infection rate. For masking, green bars represent universal masking in package and blue represents only masking around HCWs. Each individual bar = single combination of interventions. B) Predicted number of patient infections over a 12-week omicron-like period under each combination of interventions from statistical model of simulated data
A regression model on the simulated infection rates further validates these findings and identifies significant reductions in nosocomial patient infections when universal masking (β = -79,394.50, p < 0.001), masking around patients (β = -73,212.08, p < 0.001), isolation by HCWs (β = -89,522.22, p < 0.001) and, with smaller impact, reducing occupancy rates (β = -26,261.75, p < 0.001) (Table 3). A secondary analysis exploring the combined effect of the significant interventions (HCW isolation, reduced occupancy, and masking by HCWs either universally or around patients) demonstrates that isolation by HCWs has a larger effect on patient infections than a combination of masking and reducing occupancy and that combining all three interventions has the greatest effective (Table 3, Fig. 4B).
Impact of combined interventions on HCW infections: predictive modelling
For HCW infections, increased hand-hygiene alone was the least effective intervention resulting in 572,000 infections over a three-month period compared to a maximum of 206,000 infections under the most effective single intervention, isolation of symptomatic HCWs (Fig. 5A). Masking (both universal and around patients only) was also effective when HCWs do not isolate, with universal masking more effective than masking around patients (16% reduction in infections, maximum of 538,000 vs 451,000 HCWs infected). When HCWs do isolate, the difference in mask types is less pronounced and the impact appears to be related to other interventions e.g., LFD testing.
Modelled combined effects of interventions on HCWs. A) Simulated number of HCWs infected over a 12-week omicron-like period (grey bars) under package of interventions (coloured bars = interventions in package, white = intervention not in package) ordered by infection rate. For masking, green bars represent universal masking in package and blue represents only masking around HCWs. Each individual bar = single combination of interventions. B) Predicted number of HCW infections over a 12-week omicron-like period under each combination of interventions from statistical model of simulated data
Statistical modelling of the simulated infection rates identifies significant reductions in transmission associated with lateral flow testing of HCWs (β = -22,464.66, p < 0.001, Table 4) universal masking (β = -106,902.84, p < 0.001), masking around patients (β = -34,552.93, p < 0.001), and isolation of symptomatic HCWs (β = -394,655.48, p < 0.001). There is also a small association with reduced occupancy (β = -8,2090.0, p = 0.007). A further analysis exploring the impact of the three most significant interventions combined demonstrates that isolation of symptomatic HCWs alone is more impactful than masking or LFD testing combined and that a combination of universal masking, LFD testing and isolation of symptomatic HCWs is the most effective way to prevent transmission (Table 4, Fig. 5B).
Discussion
We evaluated the counterfactual impact of removing any or all of eight interventions that were implemented in NHS England hospitals over the COVID-19 pandemic on rates of nosocomial transmission to patients and HCWs in England. While highly uncertain, given the dependency on variable evidence on the effectiveness of interventions, the model results suggest that interventions in place over the COVID-19 pandemic in England prevented over 50% of potential nosocomial infections in patients and HCWs. Testing and cohorting of patients and isolation of HCWs were the most important interventions for reducing transmission to patients and HCWs preventing up to 34% (30–40%) of infections. We also identified a significant role for masking, with universal masking being more impactful than masking around patients alone (40% (30–52%) vs 17% (14–20%) reduction). Results suggest that restricting visitation could be impactful when community prevalence rates are high. Interventions were most impactful when protection from vaccines or previous infection was low at the start of the wild-type and omicron waves and had little impact in times of high immunity.
To the best of our knowledge this is the first study to attempt to quantify the impact of IPC measures over the COVID-19 pandemic in a hospital setting. A literature search conducted to parameterise the model in this study highlighted a paucity of evidence around the effectiveness of interventions such as improving hand-hygiene, as demonstrated by other studies [21], and a wide degree of uncertainty in the effectiveness of others such as masking on reducing nosocomial transmission of respiratory viruses. Further there is a lack of evidence around compliance with any interventions that were implemented. While the model used in this study includes the effect of vaccines, as administered during this period, on both patients and HCWs, we do not evaluate the impact of alternative vaccine availability or uptake. The modelling approach used in this study has previously been used to estimate the counterfactual HCW infections assuming absence of vaccines in the second wave of the pandemic and found prioritising HCWs for vaccinations was extremely important for reducing infection rates in HCWs [9].
While the baseline results are calibrated to high-quality national datasets, the scarcity of reliable evidence on the effectiveness of individual interventions (required for simulating a scenario where they are reversed) is a key challenge. While the model has been parameterised to best reflect the available data, uncertainty remains around the contribution of nosocomial and community sources of SARS-CoV-2 infection. As COVID-19 becomes an endemic disease and pressures on health systems from other seasonal respiratory pathogens increase, there is a critical need for evidence on the effectiveness of such interventions on reducing nosocomial spread in order to design efficient and effective infection prevention and control strategies.
In this study we assumed full compliance with interventions such as testing and isolating (although the compliance in studies used to parameterise masking and hand-hygiene was not reported), and the impact of reversing an intervention was applied to every interaction at every timestep that the intervention was in place. If compliance was poor or changed throughout the study period, then the modelled impact of an intervention would fall. In the absence of data on policy implementation across trusts over time, we assumed uniformity between trusts in changing behaviours according to policy guidelines. When off shift, the infection risk for HCWs was uniform, and we did not account for individual-level differences in risk of infection in the community. Further, we assumed that the effect of interventions was the same regardless of the strain on SARS-CoV-2 that was circulating at the time. We also made the assumption that it is appropriate to scale up the average results from our simulations to a national level using only numbers of beds therefore implying that all trusts were similar in terms of occupancy and admissions rates throughout the pandemic. If this was not the case, the results would need to be viewed at an individual hospital level, and although we expect the general trends to hold, the magnitude of interventions' effects may change. Similarly, for HCWs we scaled the results to a national level using total patient-facing HCW counts alone and assumed that the infection risk for staff off-shift was uniform which may not be true in reality and we could be under or overestimating the impact of interventions such as masking if staff were more or less risk-averse than the general population when off-shift. Due to policies being implemented universally and in quick succession at the start of the pandemic, there is limited opportunity to analyse their efficacy from a data-driven perspective; however, a small number of studies exist that validate the results of this modelling study. A single-site study showed that between the first and second waves the proportion of nosocomial infections in HCWs attributable to HCW-to-HCW transmission fell from 55.3% in wave 1 (01-March-2020 to 25-July-2020) to 37.4% in wave 2 (30-Nov-2020 to 24-Jan-2021) despite the proportion of community-acquired infections remaining at 50% [2]. This suggests that the introduction of masks in communal spaces in June 2020 potentially played a role in reducing HCW-to-HCW transmission by as much as 32%. This is consistent with our estimate that over wave 1 an additional 50% (27%-57%) of HCWs would have been infected had universal masking not being introduced. Another study examined the impact of removing HCW masking on patient infections and did not see a significant increase in infections when masks were removed during the first 10 months of omicron when immunity from previous infection and/or vaccination was high [22]. This agrees with simulation results where an increase in patient infections in the absence of masking was observed in the wild-type and early omicron waves, but there is little difference when vaccination and immunity from previous infection has increased protection. We did not find a notable increase in nosocomial patient infections following the withdrawal of asymptomatic testing of patients and HCWs or of masking late in 2022.
This analysis identified testing and isolation of symptomatic HCWs and masking by HCWs around both patients and other HCWs as the most important interventions for reducing infections in the patient and HCW populations. There is evidence from early in the pandemic that HCW-to-HCW transmission commonly occurred and the risk of HCW-to-patient transmission is likely small [2,3,4, 10]. However, there remains a potential for a larger effect of a small number of HCW-to-patient transmissions seeding larger outbreaks on patient wards. This cannot be ignored, and likely contributes to the increased impact of interventions that minimise HCW-to-patient transmission. However, there remains a. This impact. A strength of the IBM is that it captures these ‘knock-on’ benefits associated with prevention of transmission chains both within and across patient and HCW populations; such combined/bundled effects are sometimes referred to as the ‘Swiss Cheese’ infection prevention model [23, 24]. This cumulative effect of reducing transmissions is apparent when looking at the impact of removing all interventions in combination, which results in a higher number of nosocomial infections than the sum of the individual interventions. Model findings suggest that collectively the interventions introduced over the SARS-CoV-2 pandemic in England averted 400,000 (240,000 – 500,000) infections in inpatients and 410,000 (370,000 – 450,000) HCW infections.
Masking was found to be a highly effective intervention, but due to a lack of studies exploring the impact of different mask types we consider the overall impact of any masking in this study and do not distinguish respirators from fluid resistant surgical masks (FRSMs). A previous modelling study suggested that respirators may be advantageous for preventing infections in HCWs; however, the authors explicitly state that their study provides evidence that more work should be done to determine the true effectiveness of respirators over FRSMs [25], and no further convincing evidence has yet emerged. Analysis of intervention reversal only considered those described; additional measures such a double gloving or sessional gown use are not included in this work. The impact of interventions such as increasing bed spacing and improving ventilation were not modelled as their impact could not be included in the existing modelling framework upon which this study was conducted. While we have attempted to estimate the impact of results on infection rates, the adverse impact of interventions such as restricting visitation or mask wearing on patient care and staff wellbeing have been well documented and cannot be ignored [26,27,28,29,30,31,32,33,34,35,36]. This extensive literature should be considered alongside the results of modelling work when making future policy decisions.
Conclusion
This study combines a transmission model with published parameter estimates on the impact of individual measures to evaluate the contribution that the collection of interventions and hospital changes in place over the COVID-19 pandemic in England made to the reduction of nosocomial transmission, quantifying both individual intervention and collective impact. A strength of the modelling approach used here is the ability of the model to capture cumulative effects of interventions through reducing the seeding of new infection clusters. These results highlight the importance of maintaining high levels of compliance to infection prevention and control measures in hospitals and have important implications as hospitals prepare for a surge in demand due to emerging winter pressures and COVID-19.
Availability of data and materials
All UKHSA-held data (from SUS and SGSS as detailed in Supplementary File 1) were collected within statutory approvals granted to UKHSA for infectious disease surveillance and control. Information was held securely and in accordance with the Data Protection Act 2018 and Caldicott guidelines. The data that support the findings of this study are available from NHS Digital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The datasets used and/or analysed during the current study are however available from the corresponding author on reasonable request and with permission of NHS Digital.
References
Bhattacharya A, Collin SM, Stimson J, Thelwall S, Nsonwu O, Gerver S, et al. Healthcare-associated COVID-19 in England: A national data linkage study. J Infect. 2021;83(5):565–72.
Lindsey BB, Villabona-Arenas ChJ, Campbell F, Keeley AJ, Parker MD, Shah DR, et al. Characterising within-hospital SARS-CoV-2 transmission events using epidemiological and viral genomic data across two pandemic waves. Nat Commun. 2022;13(1):671.
Illingworth CJ, Hamilton WL, Warne B, Routledge M, Popay A, Jackson C, et al. Superspreaders drive the largest outbreaks of hospital onset COVID-19 infections. Walczak AM, Ogbunugafor CB, Cobey SE, editors. eLife. 2021;24(10):e67308.
Ellingford JM, George R, McDermott JH, Ahmad S, Edgerley JJ, Gokhale D, et al. Genomic and healthcare dynamics of nosocomial SARS-CoV-2 transmission. eLife. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8009659/. Cited 2021 May 21;10
Stimson J, Pouwels KB, Hope R, Cooper BS, Presanis AM, Robotham JV. Estimation of the impact of hospital-onset SARS-CoV-2 infections on length of stay in English hospitals using causal inference. BMC Infect Dis. 2022;22(1):1–12.
Digital NHS. Hospital Episode Statistics (HES): Provisional Monthly Statistics for Admitted Patient Care, Outpatient and Accident & Emergency. Available from: https://data.gov.uk/dataset/c914f943-98d1-4dee-aba5-c40a7d08eefa/hospital-episode-statistics-hes-provisional-monthly-statistics-for-admitted-patient-care-outpatient-and-accident-emergency. Cited 2020 May 18.
May R, Powis S. Expansion of patient testing for Covid-19. 2020.
COVID-19: infection prevention and control (IPC). GOV.UK. Available from: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control. Cited 2021 Mar 12.
Pople D, Monk EJM, Evans S, Foulkes S, Islam J, Wellington E, et al. Burden of SARS-CoV-2 infection in healthcare workers during second wave in England and impact of vaccines: prospective multicentre cohort study (SIREN) and mathematical model. BMJ. 2022;20(378): e070379.
Evans S, Stimson J, Pople D, Bhattacharya A, Hope R, White PJ, et al. Quantifying the contribution of pathways of nosocomial acquisition of COVID-19 in English hospitals. Int J Epidemiol. 2022;51(2):393–403.
Birrell P, Blake J, van Leeuwen E, Gent N, De Angelis D. Real-time nowcasting and forecasting of COVID-19 dynamics in England: the first wave. Philosophical Transactions of the Royal Society B: Biological Sciences. 1829;2021(376):20200279.
Coronavirus » Novel coronavirus (COVID-19) standard operating procedure. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/11/C0873_i_SOP_LFD-rollout-for-asymptomatic-staff-testing_phase-2-trusts-v1.1_16-nov20.pdf. Cited 2020 Dec 1.
Quilty BJ, Clifford S, Hellewell J, Russell TW, Kucharski AJ, Flasche S, et al. Quarantine and testing strategies in contact tracing for SARS-CoV-2: a modelling study. Lancet Public Health. 2021;6(3):e175–83.
May R, Powis S, Issar P, Philip P. Healthcare associated COVID-19 infections – further action. 2020. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/Healthcare-associated-COVID-19-infections--further-action-24-June-2020.pdf
Statistics » Bed Availability and Occupancy. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/. Cited 2022 Dec 21.
NHSE/I updates guidance on inpatient visiting, allowing it only “in a very careful and COVID-secure way”. COVID-19 policy tracker. Available from: https://covid19.health.org.uk/theme/nhsei-updates-guidance-inpatient-visiting-allowing-it-only-very-careful-and-covid-secure-way. Cited 2023 Jul 3.
Temime L, Gustin M-P, Duval A, Buetti N, Crépey P, Guillemot D, et al. A Conceptual Discussion About the Basic Reproduction Number of Severe Acute Respiratory Syndrome Coronavirus 2 in Healthcare Settings. Clin Infect Dis. 2021;72(1):141–3.
Face masks and coverings to be worn by all NHS hospital staff and visitors. GOV.UK. Available from: https://www.gov.uk/government/news/face-masks-and-coverings-to-be-worn-by-all-nhs-hospital-staff-and-visitors. Cited 2023 Jul 3.
Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021;11(1): e046199.
Alden K, Read M, Timmis J, Andrews PS, Veiga-Fernandes H, Coles M. Spartan: A Comprehensive Tool for Understanding Uncertainty in Simulations of Biological Systems. PLoS Comput Biol. 2013;9(2): e1002916.
Jafari Y, Yin M, Lim C, Pople D, Evans S, Stimson J, et al. Effectiveness of infection prevention and control interventions, excluding personal protective equipment, to prevent nosocomial transmission of SARS-CoV-2: a systematic review and call for action. Infect Prev Pract. 2022;4(1): 100192.
Patterson B, Mehra R, Breathnach A. Unmasking the mask: A time-series analysis of nosocomial COVID-19 rates before and after removal. In Copenhagen: ECCMID; 2023. (conference abstract).
Noh JY, Song JY, Yoon JG, Seong H, Cheong HJ, Kim WJ. Safe hospital preparedness in the era of COVID-19: The Swiss cheese model. Int J Infect Dis. 2020;98:294–6.
Yanke E, Carayon P, Safdar N. Translating evidence into practice using a systems engineering framework for infection prevention. Infect Control Hosp Epidemiol. 2014;35(9):1176–82.
Ferris M, Ferris R, Workman C, O’Connor E, Enoch DA, Goldesgeyme E, et al. Efficacy of FFP3 respirators for prevention of SARS-CoV-2 infection in healthcare workers. Elife. 2021;16:10.
Hugelius K, Harada N, Marutani M. Consequences of visiting restrictions during the COVID-19 pandemic: An integrative review. Int J Nurs Stud. 2021;121: 104000.
Mheidly N, Fares MY, Zalzale H, Fares J. Effect of Face Masks on Interpersonal Communication During the COVID-19 Pandemic. Front Public Health. 2020 Dec. Available from: https://www.frontiersin.org/articles/ https://doi.org/10.3389/fpubh.2020.582191/full. Cited 2023 Jan 10;8.
Nicholls I, Saada L. Communication, Confusion, and COVID-19: the challenges of wearing PPE on a geriatrics ward during the COVID-19 pandemic. Re: Patient perspective: Gordon Sturmey and Matt Wiltshire,. BMJ. 2023 Jan 10; Available from: https://www.bmj.com/content/369/bmj.m1814/rr. Cited 2023 Jan 10.
Bloemberg D, Musters SCW, van der Wal-Huisman H, van Dieren S, Nieveen van Dijkum EJM, Eskes AM. Impact of family visit restrictions due to COVID19 policy on patient outcomes A cohort study. J Adv Nurs. 2022;78(12):4042–53.
Aengst J, Walker-Stevenson G, Harrod T, Ivankovic J, Neilson J, Guise J-M. Uncomfortable yet necessary: The impact of PPE on communication in emergency medicine. Int J Qual Health Care. 2022 Dec 28;34(4). Available from: https://academic.oup.com/intqhc/article/34/4/mzac095/6854825. Cited 2023 Jan 10.
Muzzi E, Chermaz C, Castro V, Zaninoni M, Saksida A, Orzan E. Short report on the effects of SARS-CoV-2 face protective equipment on verbal communication. Eur Arch Otorhinolaryngol. 2021;278(9):3565–70.
Hampton T, Crunkhorn R, Lowe N, Bhat J, Hogg E, Afifi W, De S, Street I, Sharma R, Krishnan M, Clarke R, Dasgupta S, Ratnayake S, Sharma S. The negative impact of wearing personal protective equipment on communication during coronavirus disease 2019. J Laryngol Otol. 2020;134(7):577–81. https://doi.org/10.1017/S0022215120001437.
Swaminathan R, Mukundadura BP, Prasad S. Impact of enhanced personal protective equipment on the physical and mental well-being of healthcare workers during COVID-19. Postgrad Med J. 2022;98(1157):231–3.
Aloweni F, Bouchoucha SL, Hutchinson A, Ang SY, Toh HX, Suhari NAB, et al. Health care workers’ experience of personal protective equipment use and associated adverse effects during the COVID-19 pandemic response in Singapore. J Adv Nurs. 2022;78(8):2383–96.
Ayton D, Soh S-E, Berkovic D, Parker C, Yu K, Honeyman D, et al. Experiences of personal protective equipment by Australian healthcare workers during the COVID-19 pandemic, 2020: A cross-sectional study. PLoS ONE. 2022;17(6): e0269484.
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Impact of personal protective equipment use on health care workers’ physical health during the COVID-19 pandemic: A systematic review and meta-analysis. Am J Infect Control. 2021;49(10):1305–15.
Acknowledgements
We thank the experts who participated in the elicitation exercise and also the participants of model review and IPC effectiveness workshops that helped to shape the direction of this project. We also thank the SIREN team at the UKHSA for their data insight throughout the development of this model, and all those involved in running SIREN at participating sites and SIREN participants.
Disclaimer
The views expressed are those of the authors and not necessarily those of the UK Department of Health and Social Care (DHSC), FCDO, EU, MRC, NIHR, or UKHSA.
Funding
PJW was supported by the MRC Centre for Global Infectious Disease Analysis (grant number MR/X020258/1); this award comes under the Global Health EDCTP3 Joint Undertaking. PJW was also supported by the NIHR Health Protection Research Unit in Modelling and Health Economics, which is a partnership between the UKHSA, Imperial College London, and LSHTM (grant code NIHR200908). PJW has received payment from Pfizer for teaching of mathematical modelling of infectious disease transmission and vaccination, and from the Dutch National Institute for Public Health and the Environment (RIVM) for participation in an audit committee on COVID-19 data analytics and modelling.
Funding sources had no role in the design of this study.
Author information
Authors and Affiliations
Contributions
SE, JR, MW, and PW conceptualised the study, developed the methodology and interpreted the results. SE developed and parameterised the model, ran the analysis, and wrote the manuscript. JS and DP curated the data for parameterisation and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a computational study and no results using human data are reported. Data were used to calibrate the model as described in previous studies. Ethical approval and inclusion of personal data without direct consent to participate was reviewed by the United Kingdom Health Security Agency’s (UKHSA’s) governance processes, and the work was authorised to process identifiable data under Regulation 3 of Sect. 251 of the National Health Service Act 2006. No specific administrative permissions and/or licenses were acquired to access the clinical and personal patient data used in this research.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Evans, S., Stimson, J., Pople, D. et al. Impact of interventions to reduce nosocomial transmission of SARS-CoV-2 in English NHS Trusts: a computational modelling study. BMC Infect Dis 24, 475 (2024). https://doi.org/10.1186/s12879-024-09330-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09330-z